Does COPD and Emphysema Require Oxygen?
Does COPD and Emphysema Require Oxygen?

Chronic obstructive pulmonary disease, the full name is chronic obstructive pulmonary disease, people often say chronic bronchitis, emphysema all belong to the category of this disease. This is a disease in which breathing is restricted due to airway obstruction. Severe bronchial secretions lead to increased secretion, which will block the airway, cough, and expectoration.
The airway becomes narrow due to obstruction, and breathing will be restricted, causing wheezing and difficulty breathing.
If COPD is not well controlled, it will deteriorate very quickly, and when it develops to an advanced stage, there will be a state of systemic hypoxia. At this time, the doctor may recommend the patient to inhale oxygen.
However, not all patients with COPD need oxygen inhalation. Only when the disease develops to a more serious stage or when the patient does show signs of hypoxia, the doctor will advise the patient to inhale oxygen.

Which patients need oxygen?
Oxygen inhalation is recommended for blood oxygen levels below 88
In fact, what we usually call oxygen inhalation is long-term oxygen therapy. Generally speaking, long-term oxygen therapy must meet certain conditions. When the patient's arterial blood gas analysis oxygen partial pressure is lower than 55 mm Hg, or peripheral blood oxygen saturation monitoring is lower than 88, long-term oxygen therapy is recommended for the patient.
For patients without real hypoxia, doctors do not recommend that patients take oxygen at home. Because too much oxygen may produce oxygen free radicals, aggravating airway inflammation. In addition, whether it is an oxygen cylinder or an oxygen generator, there are some precautions for home use, such as fire prevention. At the same time, many COPD patients have smoking habits, which may pose potential dangers.
The lung function of patients with COPD will gradually decline. Generally speaking, oxygen therapy is the treatment method adopted when COPD develops to the advanced stage. At this time, the lung function of the patient has been seriously reduced. The role of oxygen therapy is not to improve lung function, but to prevent COPD patients from developing serious complications such as pulmonary hypertension and pulmonary heart disease due to long-term hypoxia.

For COPD patients who need long-term oxygen inhalation, how to choose the oxygen inhalation time?
For COPD patients, low-flow, low-concentration oxygen inhalation must be emphasized. Generally speaking, the flow rate of patients with COPD is below 2 liters/minute, and the flow meter of the oxygen generator has a scale, and the flow rate can be adjusted at 1 to 2 liters/minute, which is low-flow oxygen inhalation. Low-concentration oxygen inhalation means that the oxygen concentration is kept below 35%.
Oxygen concentration and oxygen flow rate are related, which can be known through the conversion relationship. Generally, the oxygen concentration of a flow rate of 3.5 liters per minute is 35%. At home, the oxygen concentration generated by the general oxygen generator is above 90%. By adjusting the oxygen flow rate, the oxygen concentration inhaled by the patient can be reduced to below 35%, which will not be pure oxygen. Low-flow, low-concentration oxygen inhalation can fully achieve the purpose of treatment.
Many people worry about whether long-term oxygen inhalation will cause oxygen poisoning. In fact, if inhaling 100% pure oxygen for a long time, it is indeed possible. However, oxygen therapy uses nasal cannula to inhale oxygen. Even if the oxygen flow rate is adjusted to the maximum, it is unlikely. Oxygen toxicity occurs. Carbon dioxide retention may occur when the oxygen concentration is too high, which means that patients with COPD inhale too much oxygen and cannot expel carbon dioxide, which is not oxygen poisoning. Therefore, doctors recommend not to increase the oxygen flow and oxygen concentration easily.
Why does COPD need an oxygen concentrator when using a ventilator?
COPD is caused by small airway blockage. As the small airway blockage becomes severe, the patient's gas exchange will become difficult. At this time, hypoxia and carbon dioxide retention will occur.
Using a ventilator can improve the patient's ventilation. For example, before using the ventilator, only 100 ml of gas can be exchanged per breath. After using a ventilator with a circuit, it can exchange 400 ml of gas each time, so in theory, air can be inhaled every time. Increased, then the patient's hypoxia-like symptoms should improve, but the actual situation is that the patient needs to be connected to the oxygen generator while using the ventilator, so why?

COPD hypoxia is mainly due to impaired diffusion
The hypoxia in COPD patients is mainly due to the damage of the alveolar diffusion function. The so-called diffusion function is the function of oxygen in the alveoli entering the blood. It can be simply understood as a problem in the ability of COPD patients to absorb oxygen.
The air inhaled into the lungs finally undergoes gas exchange in the alveoli. The alveoli are surrounded by capillaries. The capillaries and alveoli are separated by a layer of "breathing membrane". This membrane is extremely thin and is very conducive to the oxygen in the alveoli. Entering the blood, colleagues blood carbon dioxide enters the alveoli through this membrane.
Due to the blockage of small airways in COPD, the alveoli will retain gas and expand, and some alveoli will fuse with each other, which will lead to bullae or emphysema, which will lead to a decrease in the volume of the respiratory membrane, resulting in obstacles to oxygen exchange.
In this case, even if the patient inhales as much air as us normal people, due to the problem of absorption, it is necessary to increase the oxygen concentration to improve the hypoxia situation.
The diffusion rate of carbon dioxide is 20 times that of oxygen. Carbon dioxide can easily pass through the alveoli from the middle of the respiratory membrane. This is why COPD is dominated by hypoxia in the early stage, and only in the later stage does carbon dioxide retention occur. The reason is carbon dioxide retention. As long as the respiratory function is still good, then generally there will be no problem of not being able to discharge carbon dioxide.

Because the patient's ability to exchange gas is too low for spontaneous breathing, there is always a part of carbon dioxide that cannot be excreted from the body, so after accumulation, the carbon dioxide in the body will increase. Therefore, after such patients use the ventilator, the ventilator can improve the ventilation capacity, so that The carbon dioxide in the alveoli can be expelled with exhalation.
The function of the oxygen concentrator is to increase the oxygen concentration, and the ventilator expels carbon dioxide in the alveoli by enhancing the ventilation capacity. The oxygen concentrator allows more oxygen to enter the blood by increasing the oxygen concentration of the inhaled air.
Appropriately increasing the PEEP (EPAP of non-invasive ventilator) pressure of the ventilator can improve the oxygenation of the patient. This is because appropriately increasing the PEEP pressure can increase the alveolar-arterial oxygen partial pressure difference, because the greater the partial pressure difference, the lower the ventilation volume. bigger.

DEDAKJ Oxygen Concentrator
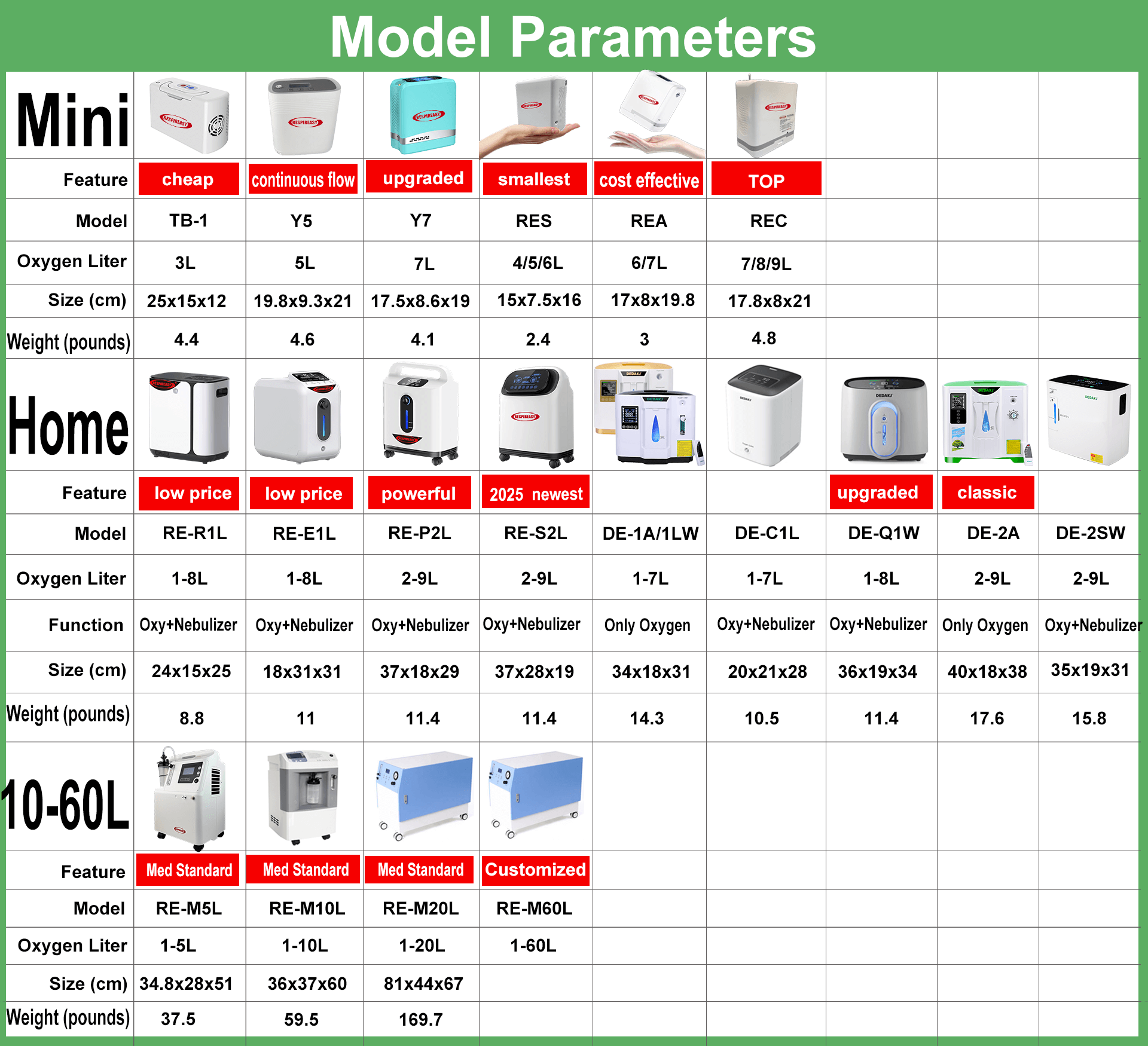
Established in 1953, with ISO, CE, RoHS and PSE certifications, with medical oxygen concentrators and home oxygen breathing machines as the core, DEDAKJ is the top-rated oxygen concentrator supplier,offers the mini &small oxygen concentrator, household portable oxygen making machine, the medical grade 10 liter oxygen concentrator for hospitals &clinics oxigenoterapia. More The DEDAKJ Oxygen Concentrator store website offers the DEDAKJ original oxygen accessory oxygen parts & components. All DEDAKJ oxygen machine oxygen concentrators concentrador de oxigeno and original oxygen accessories parts can be bought here.
Buy online the best quality portable oxygen concentrator in DEDAKJ oxygen concentrator store.